Coronary Artery Disease
Coronary heart disease is a common term for the buildup of plaque in the heart’s arteries that could lead to heart attack. But what about coronary artery disease? Is there a difference? The short answer is often no — health professionals frequently use the terms interchangeably.
Plaque refers to the buildup of fats, cholesterol and other substances in and on your artery walls. (It is also called “atherosclerosis”.) Plaque first grows within the walls of the coronary arteries until the blood flow to the heart’s muscle is limited. This is also called ischemia.
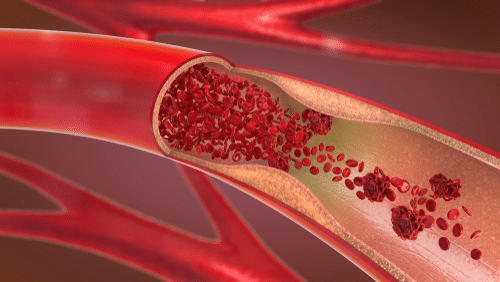
It may be chronic – narrowing of the coronary artery over time and limiting of the blood supply to part of the muscle.
Or it can be acute – resulting from a sudden rupture (or loosening) of a plaque and formation of a thrombus or blood clot. This can cause a heart attack – also called a Myocardial Infarction (MI).
How is Coronary Artery Disease detected?
At San Tan Cardiovascular, we have many ways of detecting coronary heart diseases. Arteriosclerosis is diagnosed through various tests including:
- Coronary Angiography — Coronary angiography, also called cardiac catheterization, is a minimally invasive study that is considered the gold standard for diagnosing coronary artery disease. This test is performed under local anesthesia and involves injecting X-ray dye or contrast medium into the coronary arteries via tubes called catheters. An X-ray camera films the blood flow to show the location and severity of artery narrowing. This test can show if the blood vessels in your heart have narrowed or if your heart is pumping normally and blood is flowing correctly and your heart valves are functioning properly. It also can identify any heart abnormalities you may have been born with or congenital abnormalities. If you have a blockage that requires treatment, a balloon can be pushed through the catheter and inflated to improve the blood flow in your coronary arteries. A mesh tube (stent) may then be used to keep the dilated artery open.
- CT Angiography – CT angiography uses a CT scanner to produce detailed images of both blood vessels and tissues in various parts of the body. During the exam, contrast material is injected through a small catheter placed in a vein of the arm. A radiologic technologist will capture high-resolution CT images while the contrast material flows through the blood vessels.
- Echocardiogram (ECHO) — This non-invasive test translates sound waves from your chest into pictures of your heart. It provides information about how the heart is pumping, how blood flows in the heart and blood vessels, how large the heart is and how the valves are working.
- Electrocardiogram (ECG or EKG) — The electrocardiogram records the heart’s electrical activity. Small patches called electrodes are placed on your chest, arms and legs, and are connected by wires to the ECG machine. Your heart’s electrical impulses are translated into a wavy line on a strip of paper, enabling doctors to determine the pattern of electrical current flow in the heart and to diagnose arrhythmias and heart damage.
- Stress Echocardiogram — Stress tests are performed to see how the heart performs under physical stress. The heart can be stressed with exercise on a treadmill or in a few instances, a bicycle. If you can’t exercise on a treadmill or bicycle, medications can be used to cause the heart rate to increase, simulating normal reactions of the heart to exercise. During the stress test, you will wear ECG electrodes and wires while exercising so that the electrical signals of your heart can be recorded at the same time.
- Nuclear Stress Test — Nuclear Stress Tests have two components — exercise portion and a rest portion. The patient will receive an injection of a radionuclide “tracer” material, such as Thallium or Sestamibi. This tracer will “attach” to the heart muscle and allow the doctors to see the coronary arteries and the shape and function of the heart muscle. It has been used in this manner safely for many years to demonstrate the amount of blood the heart is getting under various conditions — rest and stress.
Treatment for Coronary Artery Disease at San Tan Cardiovascular Center
At San Tan Cardiovascular Center, we have a team of highly experienced Cardiologists, Nurse Practitioners and staff to test, detect and treat you for coronary artery disease.
Treatment for coronary artery disease usually involves lifestyle changes and, if necessary, drugs and certain medical procedures. Various drugs can be used to treat coronary artery disease or to help stop the progression of the disease, including:
- Cholesterol-modifying medications. By decreasing the amount of cholesterol in the blood, especially low-density lipoprotein (LDL, or the “bad”) cholesterol, these drugs decrease the primary material that deposits on the coronary arteries.
- Aspirin. Your doctor may recommend taking a daily aspirin or other blood thinner. This can reduce the tendency of your blood to clot, which may help prevent obstruction of your coronary arteries.If you’ve had a heart attack, aspirin can help prevent future attacks. There are some cases where aspirin isn’t appropriate, such as if you have a bleeding disorder or you’re already taking another blood thinner, so ask your doctor before starting to take aspirin.
- Beta blockers.These drugs slow your heart rate and decrease your blood pressure, which decreases your heart’s demand for oxygen. If you’ve had a heart attack, beta blockers reduce the risk of future attacks.
- Calcium channel blockers.These drugs may be used with beta blockers if beta blockers alone aren’t effective or instead of beta blockers if you’re not able to take them. These drugs can help improve symptoms of chest pain.
- Ranolazine (Ranexa).This medication may help people with chest pain (angina). It may be prescribed with a beta blocker or instead of a beta blocker if you can’t take it.
- Nitroglycerin tablets, sprays and patches can control chest pain by temporarily dilating your coronary arteries and reducing your heart’s demand for blood.
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs).These similar drugs decrease blood pressure and may help prevent progression of coronary artery disease.
Procedures to restore and improve blood flow
Sometimes more aggressive treatment is needed.
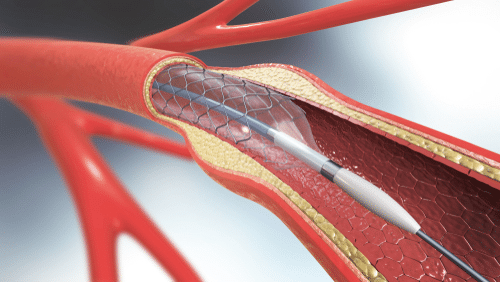
Balloon Angioplasty and Stent Placement
Your doctor inserts a long, thin tube (catheter) into the narrowed part of your artery. A wire with a deflated balloon is passed through the catheter to the narrowed area. The balloon is then inflated, compressing the deposits against your artery walls.
A stent is often left in the artery to help keep the artery open. Most stents slowly release medication to help keep the arteries open.
Coronary Artery Bypass surgery (CABG)
A surgeon creates a graft to bypass blocked coronary arteries using a vessel from another part of your body, usually your leg vein. This allows blood to flow around the blocked or narrowed coronary artery. Because this requires open-heart surgery, it’s most often reserved for cases of multiple narrowed coronary arteries.
How do I get started?
Contact San Tan Cardiovascular Center today to make an appointment with one of our healthcare providers.
At this appointment:
- we will review your medical history, discuss your symptoms and perform a non-invasive, diagnostic test to further determine your medical condition,
- any pertinent testing that needs to be done beforehand will also be ordered at this time.
Our billing department will then contact your health insurance company to obtain prior authorization. Upon receiving insurance authorization, the treatments will be scheduled.
Coronary Artery Disease FAQs
Q: What are the risk factors for coronary artery disease (cad)?
- High LDL cholesterol, low HDL cholesterol
- High blood pressure (Hypertension)
- Family history of heart problems
- Diabetes
- Smoking
- Women who are post-menopausal
- Men over 45 years old
- Obesity
Q; What are the symptoms of coronary artery disease?
- Chest pain (angina)
- shortness of breath
- sweating
- weakness
- dizziness
- nausea
- rapid heartbeat
- palpitations — the feeling that your heart is pounding hard and rapidly and is fluttering or skipping beats
Q: How do I prevent coronary artery disease?
A: Living a healthy lifestyle that incorporates:
- good nutrition – eating a healthy, balanced diet
- weight management
- getting plenty of physical activity
- quit smoking
- reduce stress
- regular annual check-ups with your primary physician
All of these can play a big role in avoiding and preventing CAD.